2012-24
Standardized and Electronic Prior Authorization
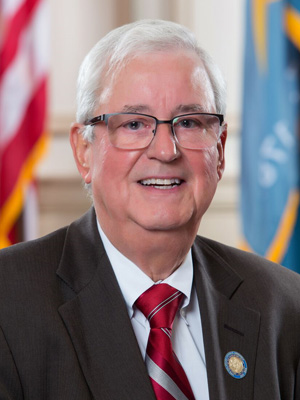
AS AMENDED REPRESENTATIVE JOSEPH E. MIRÓ (DE) INTRODUCED NATIONAL SUMMIT HEALTH CARE TASK FORCE
WHEREAS, prior authorization is a process in which physicians must seek approval from health plans for medications, diagnostic tests, and procedures needed by their patients; and
WHEREAS, physicians typically wait several days to receive authorization from an insurer for medications; and
WHEREAS, patients suffer as access to needed drugs, including pain management and chronic care medication, is delayed; and
WHEREAS, in addition, administrative tasks including prior authorization cost the health care system $23.2 to $31 billion a year; and
WHEREAS, phone calls and fax communications between pharmacies and physician offices account for up to 25% of pharmacists’ time and 20% of the workload of physician-office staff; and
WHEREAS, the current, paper-based system of prior authorization is cumbersome and administratively burdensome for providers and patients alike, in part because information requirements are inconsistent and vary by payer; and
WHEREAS, a standardized prior authorization process would mean prescribers could use the same form for all payers, saving prescribers and patients, time and money; and
WHEREAS, in addition, standardizing prior authorization would simplify the process and enhance efficiency in preparation for electronic systems; and
WHEREAS, three-quarters (75%) of physicians said an automated pre-authorization process would help them manage patients’ care more efficiently; and
WHEREAS, electronic prescribing (eRx) technology can be used to alert a prescriber of the need for prior authorization at the point of care and before completing the prescription, streamlining the process and making it more efficient; and
WHEREAS, state Medicaid programs that have implemented automated prior authorization systems, report significant cost savings as a result; and
WHEREAS, various state Departments of Health have concluded that implementation of authorization systems also present logistical challenges due to the complexity of these systems; and
WHEREAS, states ought to be afforded federal resources to implement these improvements to avoid the creation of an unfunded mandate;
THEREFORE BE IT RESOLVED, that standardized and electronic prior authorization should be required and implemented in order to improve patient care, enhance patient/provider decision making, save health care providers and patients, time and money, and increase health system efficiency and cost savings.
THIS RESOLUTION WAS ADOPTED AND RATIFIED ON NOVEMBER 17, 2012 AT THE NHCSL ANNUAL MEETING HELD IN ALBUQUERQUE, NEW MEXICO.
Sponsored by: Representative Joseph E. Miró (DE)
