Drug Pricing
Presentations will be held in May and December 2019. We encourage that legislators refrain from any policy-making on drug pricing until Decemeber.
Biopharmaceutical innovation is for everyone regardless of color, class or ability to pay. The National Hispanic Caucus of State Legislators maintains that due to the systemic history of issues pertaining to healthcare access that certain communities based on their zip code have more difficulty accessing healthcare.
A chart listing the advancements in biopharmaceutical innovations split in half. Then we had medicines made of chemical compounds, medicine that treat broad diseases, radiation and chemotherapy to treat cancer.
Public policy should recognize and reward risk taking.
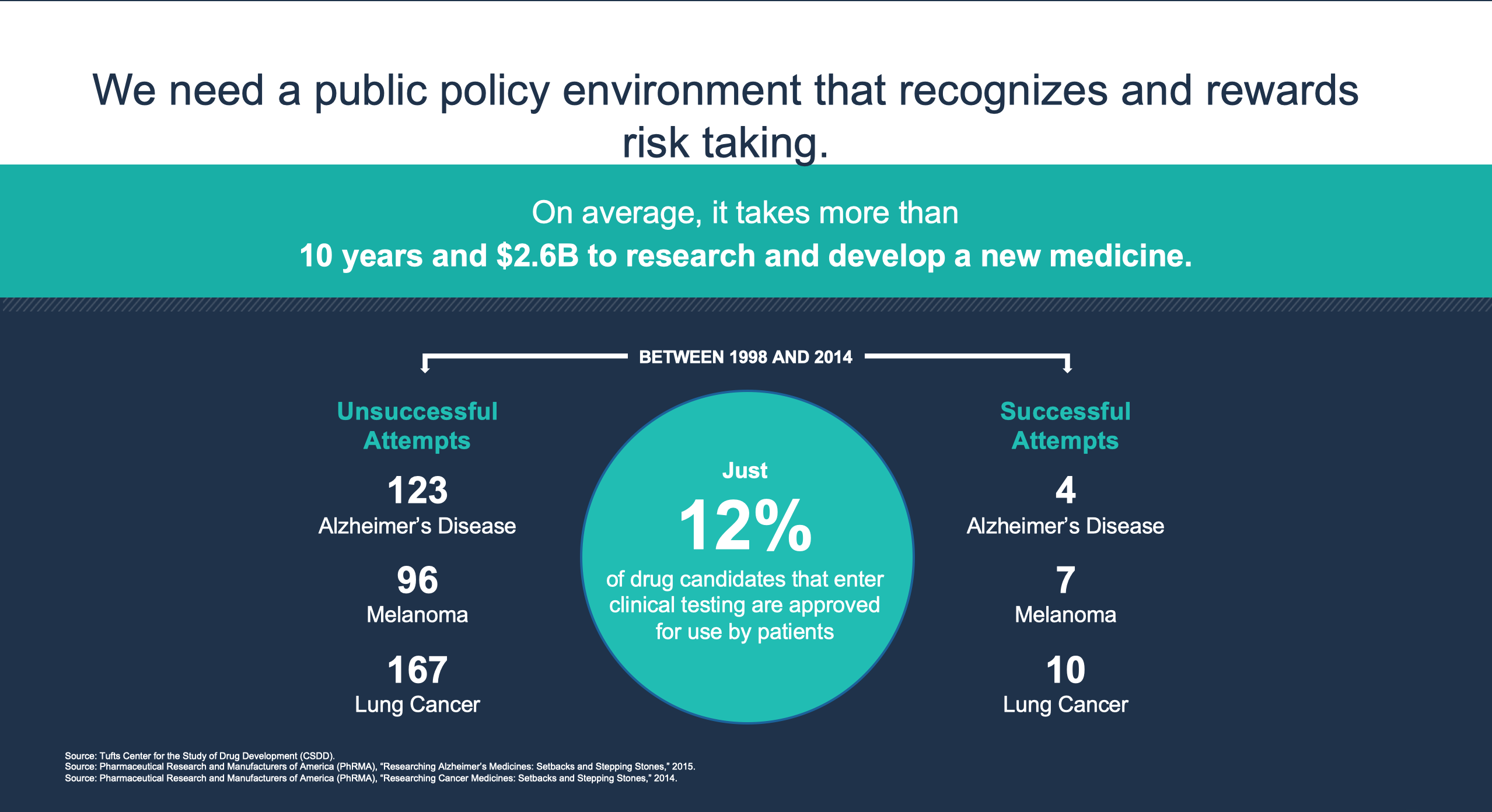
On average it takes more than 10 years and $2.6B to research and develop new medicine. Between 1998 and 2014 only 12% of drug candidates that enter clinical testing are approved for use for patients. These include 123 unsuccessful attempts at developing drugs for Alzheimer's Disease v. 4 successful. 96 v. 7 for Melanoma, and 167 for lung cancer vs. 10. This is according to sources such as Tufts Center for the Study of Drug Development, Pharmaceutical Research & Manufacturers of America. Titles include: "Researching Alzheimer's Medicines: Setbacks and Stepping Stones" (2015) and "Researching Cancer Medicines: Setbacks and Stepping Stones" (2014)
Medicine cost growth is also declining.
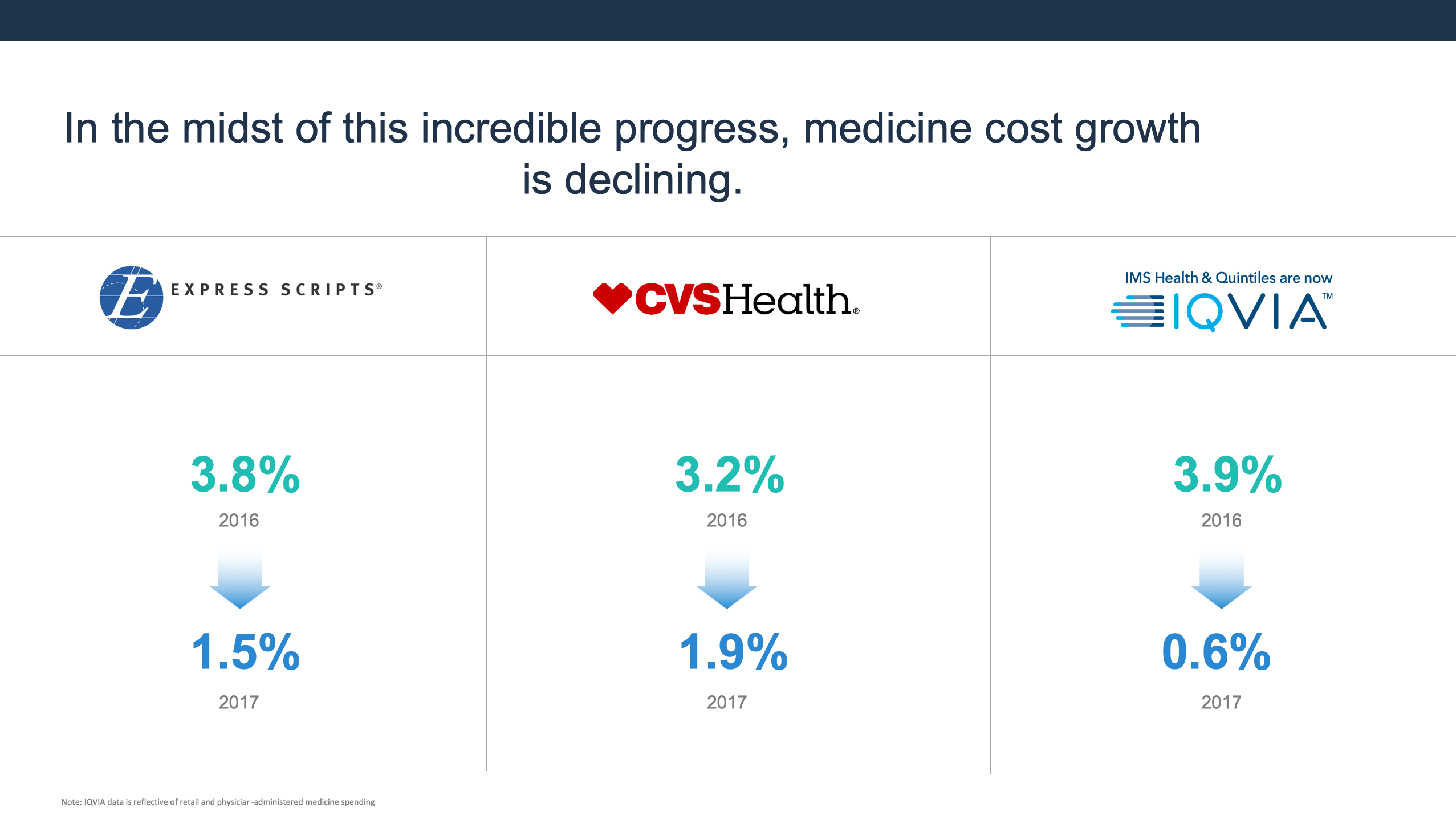
Cost growth is declining in the midst of this progress. Declines have been reported by pharmaceutical companies including ExpressScripts, CVS Health, and IQVIP. ExpressScripts reported a drop from 3.8% to 1.5%. CVS Health reported a 3.2% drop to 1.9 %, and Health IQVIP reported a drop from 3.9% to 0.6%.
According to a March 2019 IMS Health Drug Channels Institute study and a 2018 Drug Savings in the U.S. Report by the Generic Pharmaceutical Association, between 2008 and 2017, consumers $1.79 trillion by purchasing generic drugs.
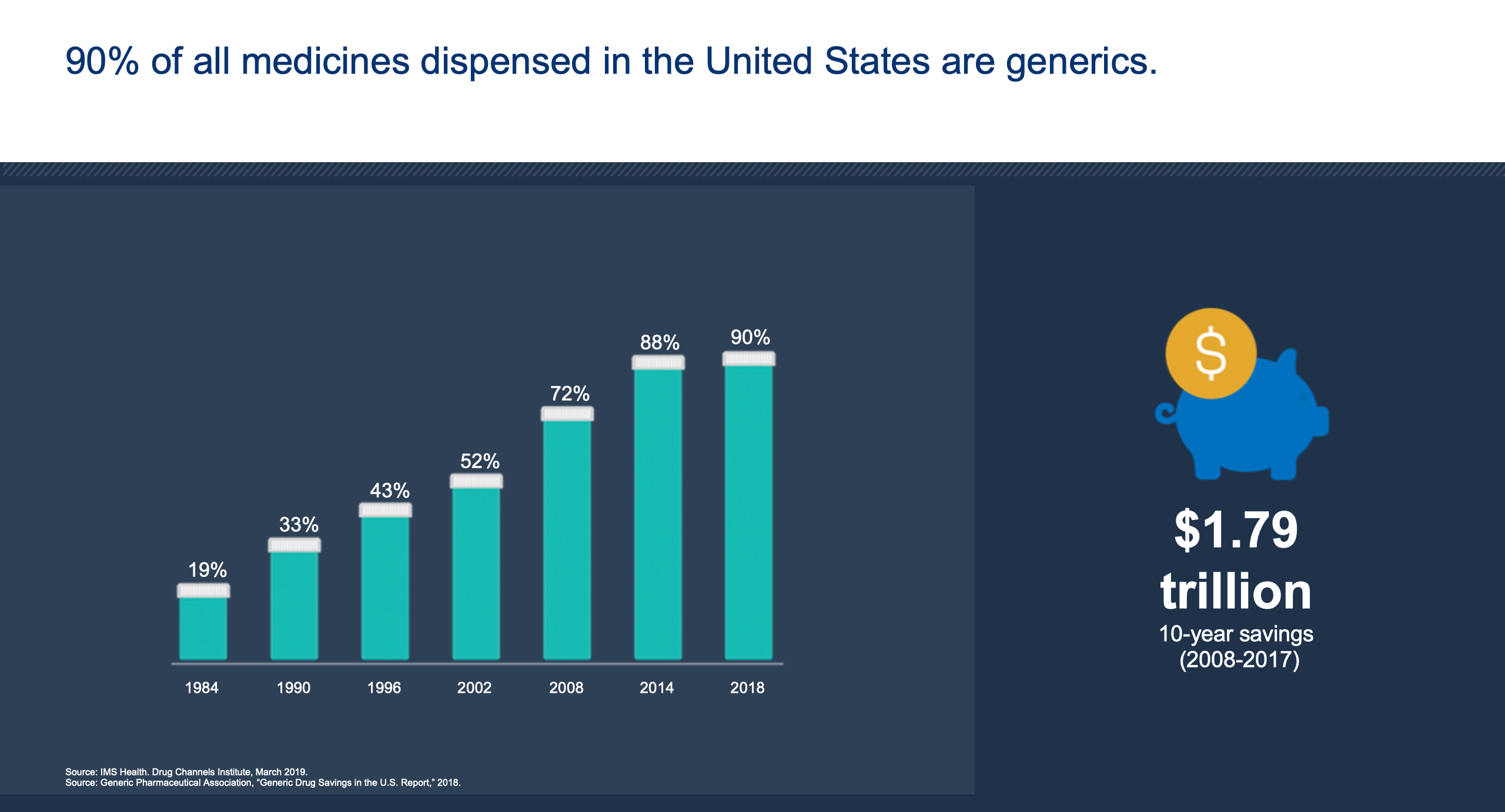
Between 2007 and 2018, $1.79 trillion was saved by using generic drugs. This is according to a 2019 IMS Health Drug Channels Institute study and a Generic Drugs Savings in the U.S. Report 2018 conducted by the Generic Pharmaceutical Association.
Insurers and Pharmacy Benefit Managers (PBMs) have a lot of leverage to hold down medical costs. Insurers determine formulary, tier placement, accessibility, and provider incentives.
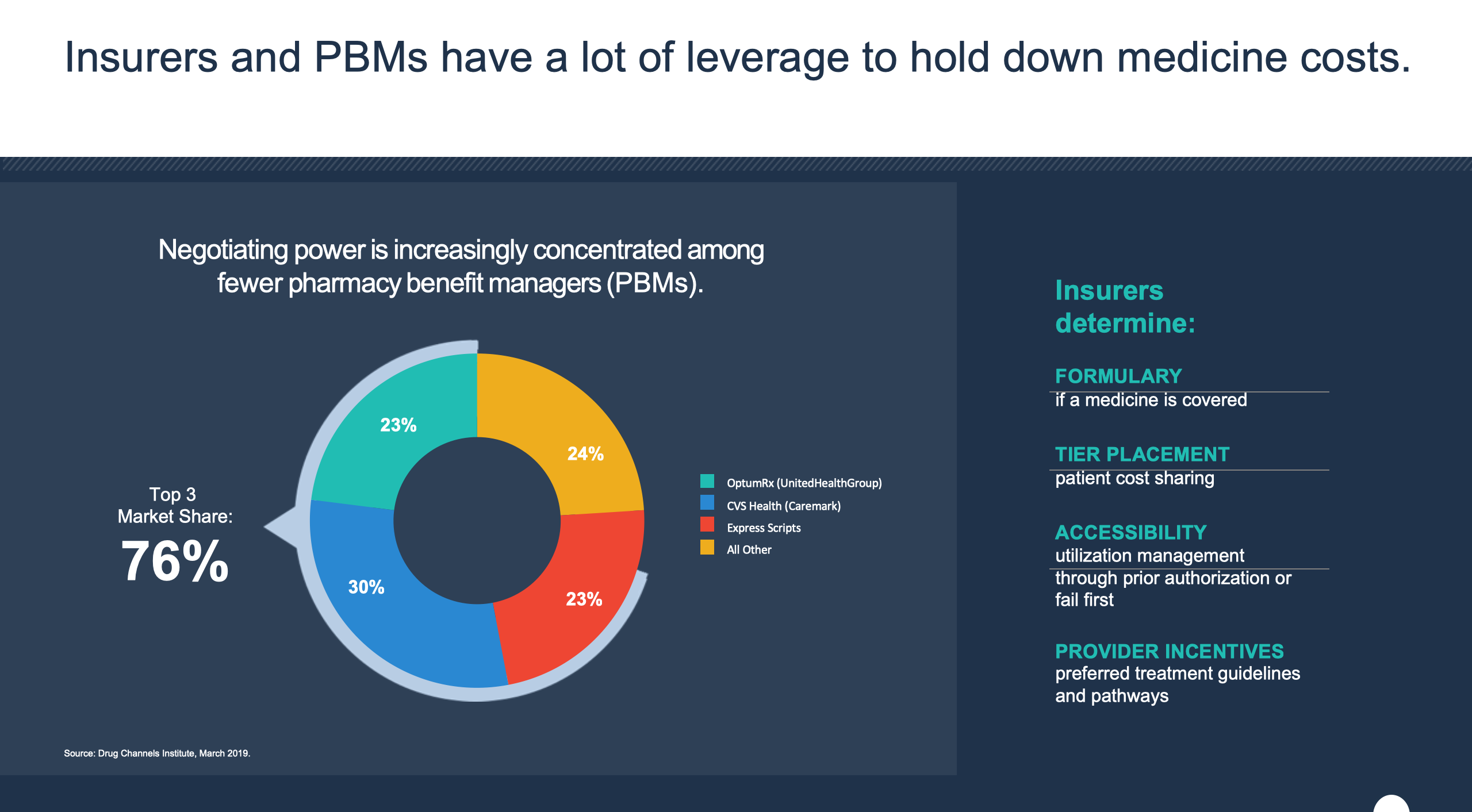
ExpressScripts, CVS Health (Caremark), and OptumRx (United Health Group) together hold approximately 76% of the market share.
Pharmaceutical drug costs have risen exponentially.
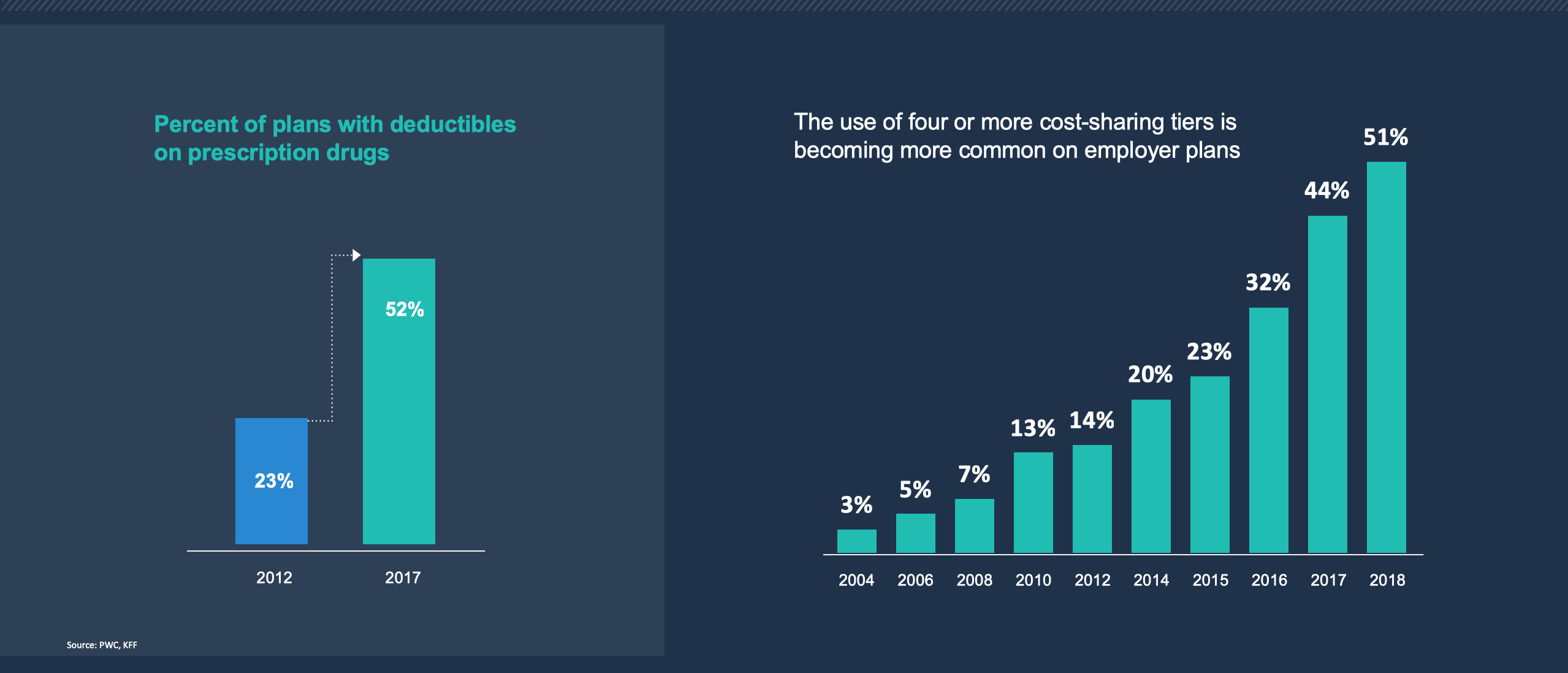
Patients in the United States are facing rising out-of-pocket costs and other barriers to education.
These costs tremendously impact the health and well-being of all Americans.
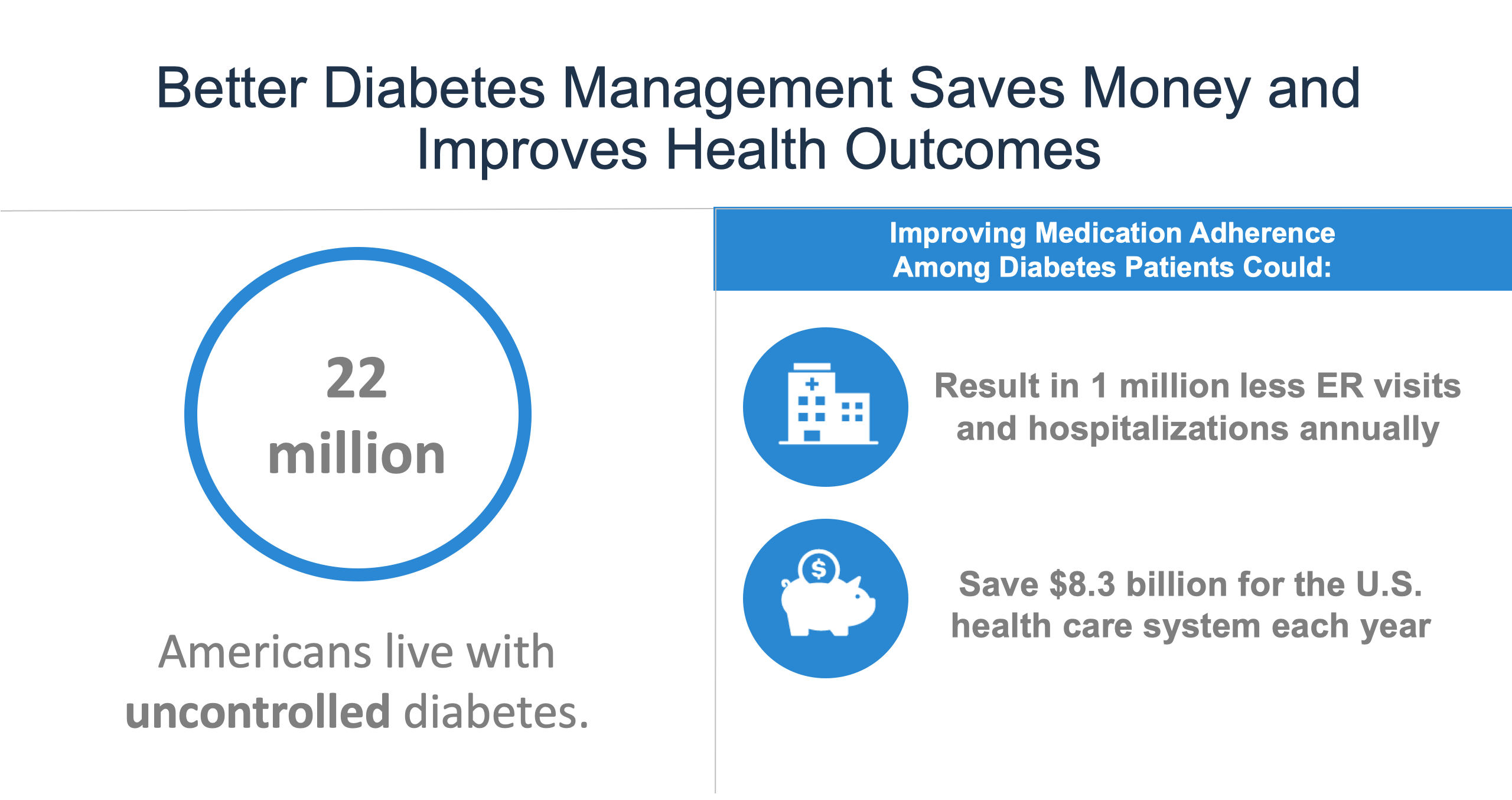
According to the American Diabetes Association and Health Affairs' "Greater Adherence to Diabetes Drugs is Linked to Less Hospital Use and Could Save Nearly $5Billion Annually," there are 22 million Americans living with uncontrolled diabetes.
According to the aforementioned studies, improving medication adherence alone among patients can have tremendous positive impacts. This includes 1 million less ER visits and hospitalizations annyally. 8.3 billion dollars would also be saved in the American healthcare system.
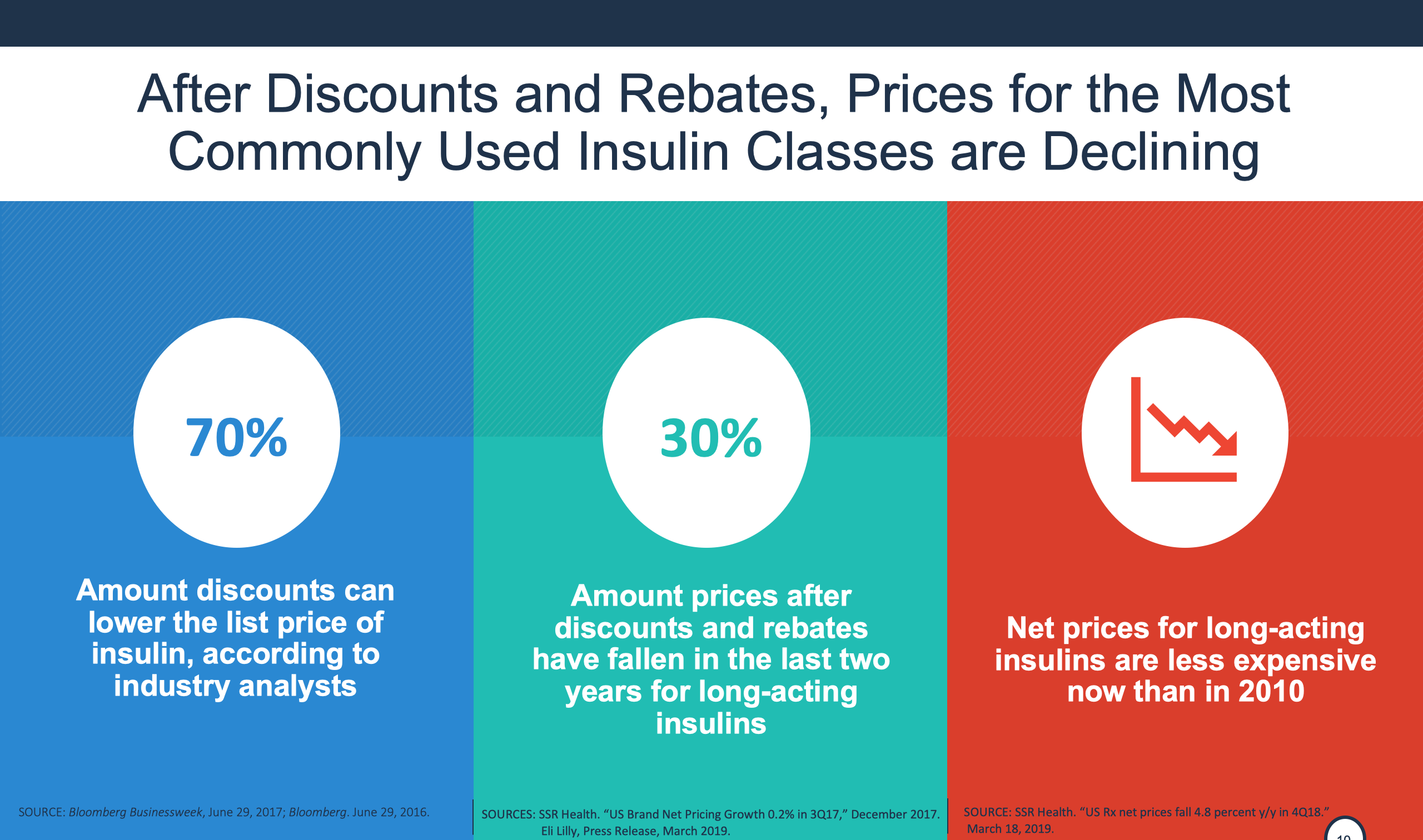
After the discounts and rebates, the most common insulin classes are experiencing price drops. According to Bloomsburg BusinessWeek, 70% amount discounts can lower list price of insulin, according to industry analysts. According to March 2019 March SR Health 30% of amount prices after discounts and rebates have fallen in the last two years for long-acting insulins. According to the March 2018 SSR Health net prices for long-acting insulin are less expensive now than they were in 2010.
Diabetes patients face soaring out-of-pocket costs.
Collective efforts must be made to alleviate the price of drugs that American consumers are paying. First, we must modernize the FDA to keep up with scientific discovery and development process. We should next promote value-driven healthcare by removing barriers restricting information that companies share with insurers. Reform regulations discouraging companies offering discounts tied to outcomes, and modifying Medicaid best pricing options. We must empower consumers and lower out-of-pocket costs. This can include: provide negotiating rebates, addressing affordability challenges in the copay, and make more information about out-of-pocket healthcare costs available to patients. We must also address the burdensome 340B Drug Pricing program regulations and improve trade agreements by insuring they recognize the value in innovating medicines.
Sharing rebates can actually improve health while lowering costs according to Candace DeMatteis, MPH and JD.
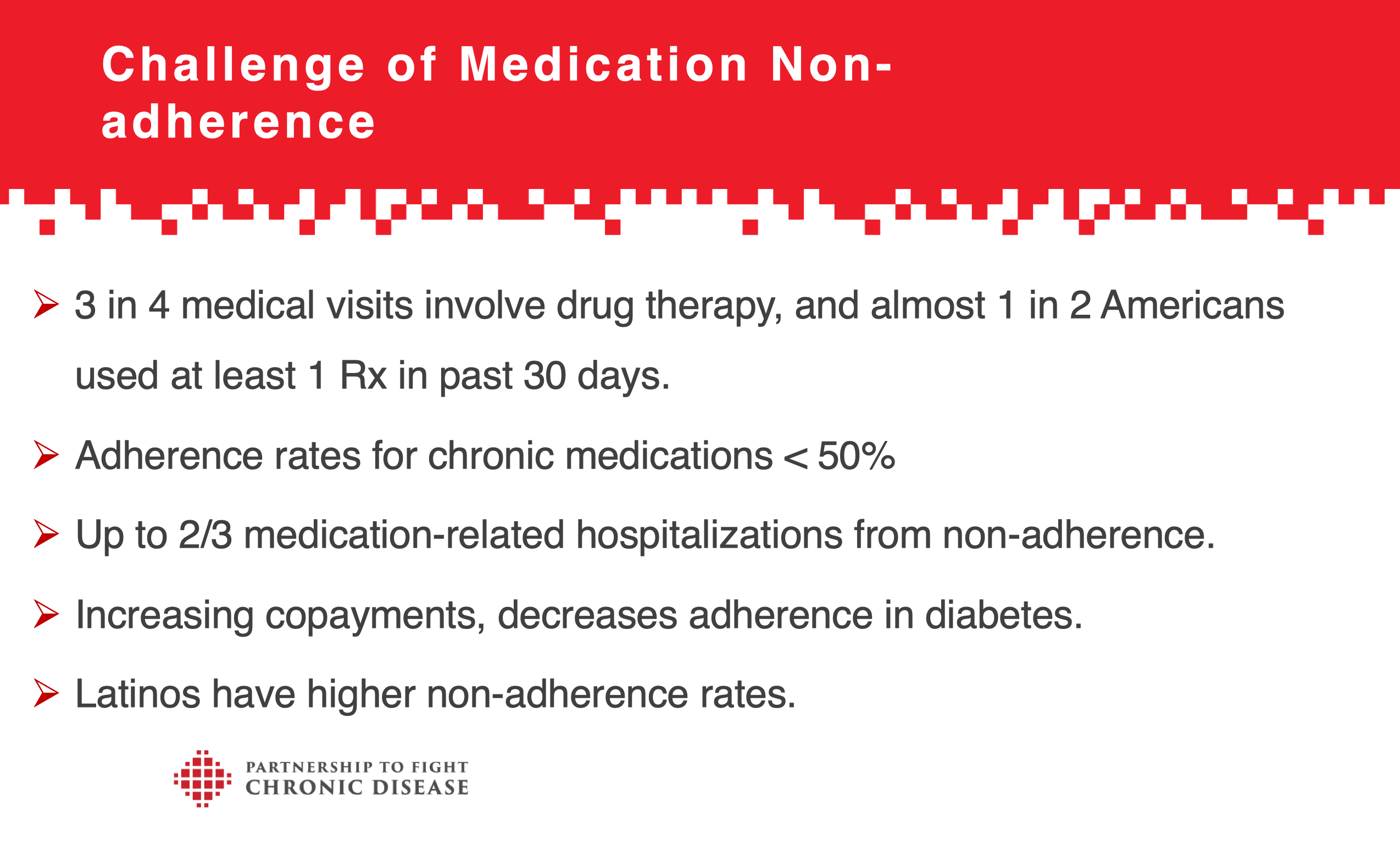
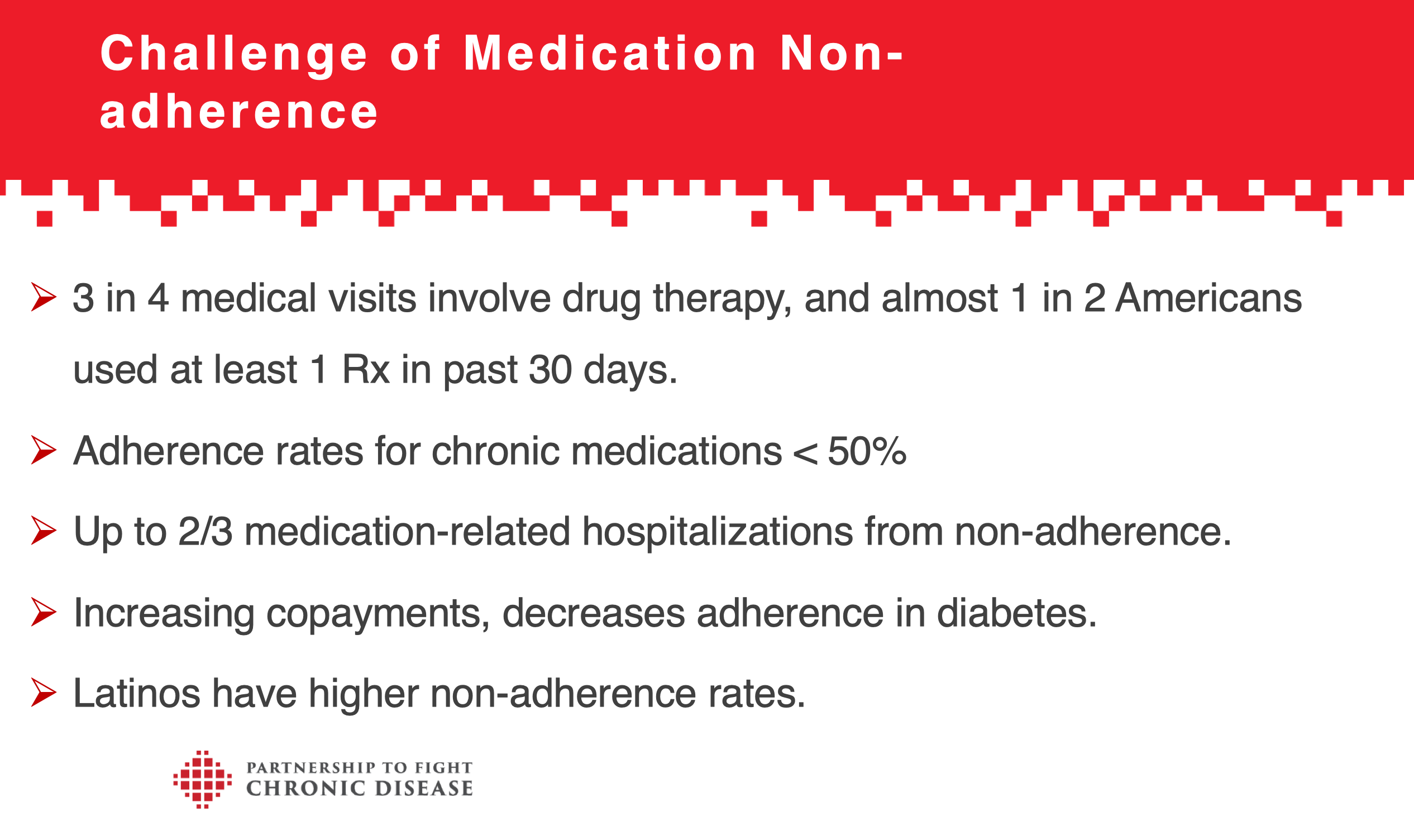
3 in 4 medical visits involve drug therapy and 1 in 2 Americans used a kind of prescription drug in the past 30 days. Adherence rates for chronic conditions is less than 50%. Up to 2/3 of medication hospitalization come from non-adherence. Increasing copayments decreases adherence in diabetes. Latinos have higher non-adherence rates.
These issues have tremendous impacts on the Latino community due to high medical nonadherence.
Sharing rebates helps everyone including people with diabetes, employers, and healthplans.
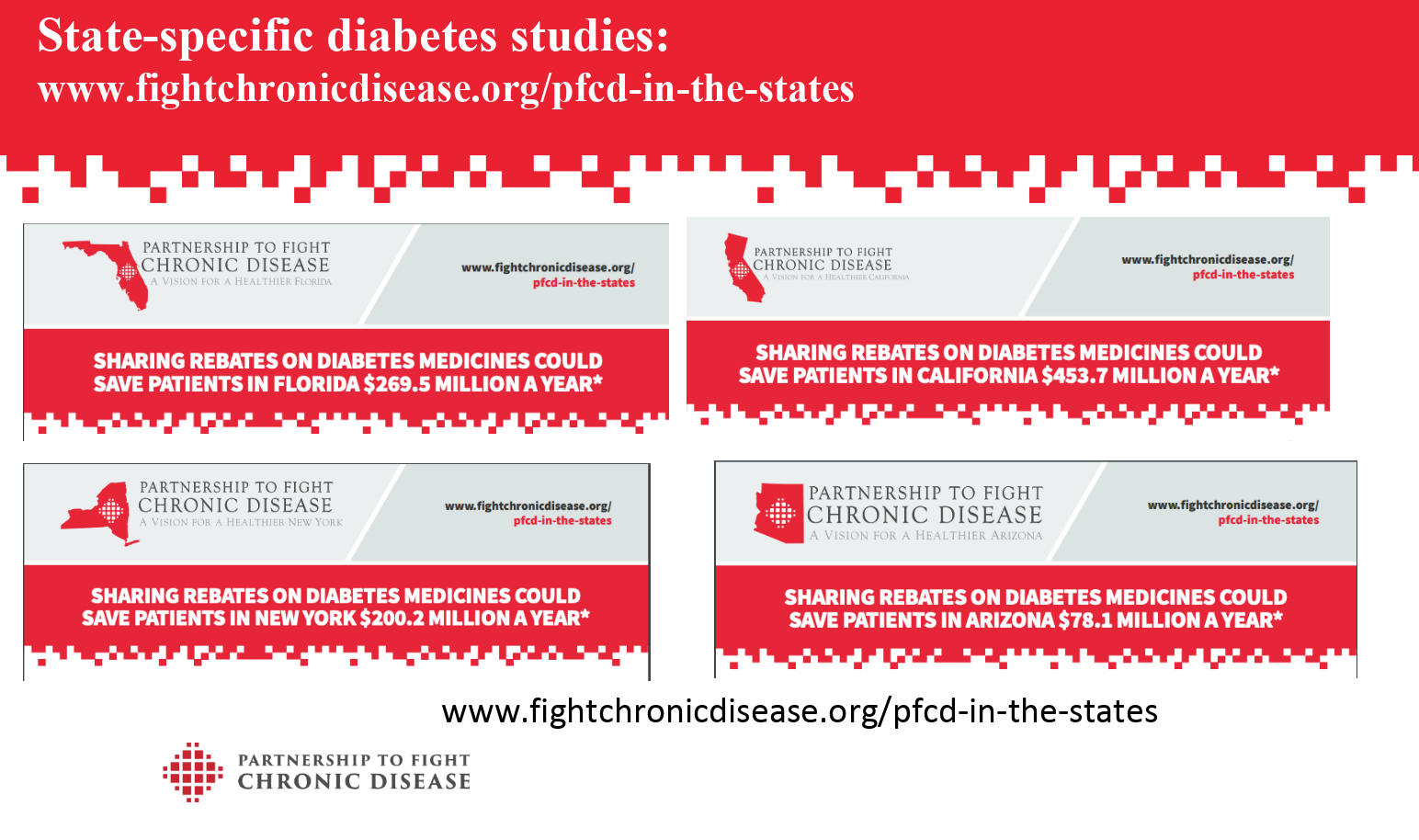
Sharing rebates on diabetes medicines could save patients in Florida $269.5 million a year. Sharing rebates on diabetes medicines could save patients in California $453.7 million a year. Sharing rebates on diabetes medicines could save patients in New York $200.2 million a year. Sharing rebates on diabetes medicines could save patients in Arizona $78.1 million a year.
Diabetes and Insulin. Over 30.3 million Americans have diabetes. 1.5 million Americans are diagnosed with diabetes every year. Diabetes cost the US $327 billion in 2017. Healthcare costs for Americans with diabetes are 2.3x greater. Over 8 million people with diabetes rely on insulin to keep their blood sugar in range (including 2.3 million people on Medicare). 1 in 4 insulin using people with diabetes have rationed their insulin according to Herkert, D, Vijayakumar, P & Luo, J of JAMA Intern Med.
How does the Rebate System work? How did we get here?
In 2003 the Medicare Prescription Drug, Improvement, and Modernization Act (MMA) created Part D for Prescription Drug coverage, Private stand-alone prescription drug plans (PDPs), Medicare Advantage drug plans (MA-PDs). Only insurance companies can administer the Medicare prescription drug program and negotiate drug pricing with manufacturers (Pharmacy Benefit Managers (PBM), MMA prohibits CMS for negotiating drug prices.
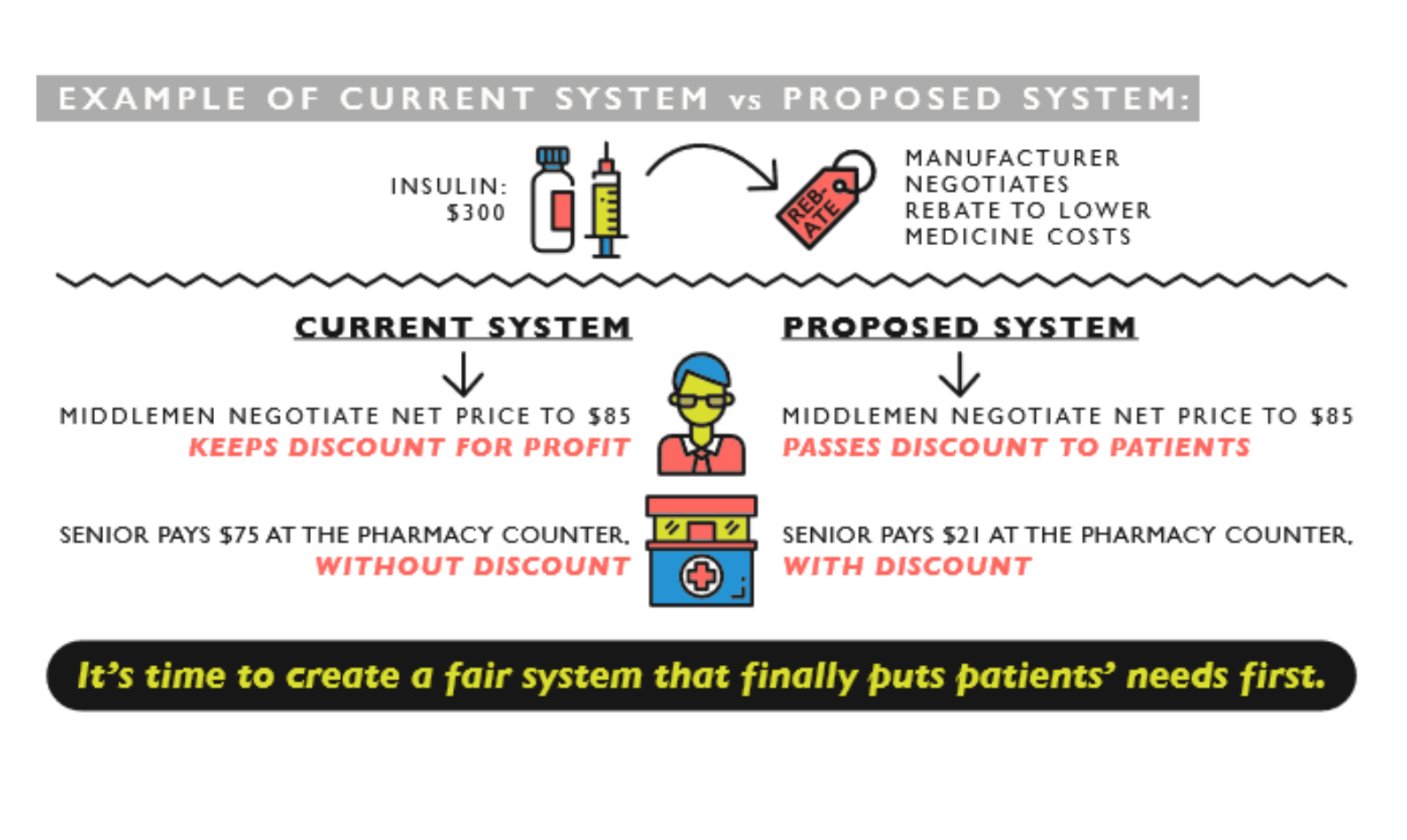
Let's say that the price of insulin is $300, and the manufacturer negotiates rebate to lower medicine costs. In the current system the middlemen negotiate the price down to $85 and keep the discount for profit. The senior pays $75 at the pharmacy counter, without discount. Under the proposed system, middlemen negotiate the price down to $85 and the discount is given to the patients. The senior pays $21 at the counter with discount....It's time to create a fair system that puts patients' need first.
The increase in the 2020 Part D premiums ranged from $3.20 to $5.64 per beneficiary per month. Under CMS actuary analysis, the majority of beneficiaries would see an increase in their total out-of-pocket payments and premium costs; reductions in total cost sharing will exceed total premium increases.
